

At one time, all brainstem gliomas were thought to be one single entity. As medicine evolved developing more sophisticated imaging with MRIs, it was found that brainstem gliomas were not all the same. Tumors in the brainstem can be located in the cervicomedullary junction, the midbrain, the tectum or the pons. Brainstem tumors can be further categorized as either diffuse intrinsic or nondiffuse. Non diffuse brainstem tumors may also be described as dorsal or exophytic. In addition, advanced neurosurgical techniques have allowed some to enter this previously considered “inoperable” area. Although the vast majority of lesions appearing as diffuse pontine gliomas by MRI are high grade, it has been found that there may be other pathology (particularly low grade glioma).
The important point – when one is looking at information (other children’s websites, journal articles, etc) it is critical to realized what kind of tumor is being discussed.
Not all brainstem gliomas are created equal.
Brainstem gliomas at other locations may have different statistics.
Diffuse instrinsic pontine gliomas have a bleaker prognosis than focal brainstem lesions.
The brainstem, of which the pons is the upper part, has three main functions,
The Lily LaRue Foundation is totally dependent on its volunteers, sponsors and donations to be able to support projects. Help us reach our goal and get involved by making a donation, volunteering, or shopping at our store.
Please click on the "Shop" tab to make a purchase or the "Donation" tab to make a tax-deductible donation to the Lily LaRue Foundation, a 501(c)(3) tax-exempt non-profit organization.
NO DONATION IS TOO BIG OR TOO SMALL.
Donations made to the Lily LaRue Foundation go toward helping DIPG families in need and supporting medical facilities and scientific trials at the forefront of their field who are specifically researching cures for Pontine Glioma.
A diffuse pontine glioma or brainstem glioma is a high-grade, or malignant, tumor. This type of tumor arises in the glial (supportive) tissue of the lowest, stem-like part of the brain, which controls many vital functions. Diffuse pontine gliomas account for 10-15 percent of all childhood central nervous system tumors, with approximately 300 new cases diagnosed in the United States each year. The median age at diagnosis is 5 to 9 years old, and these tumors occur with equal frequency in boys and girls. All children diagnosed with the disease die, typically within 3-18 months. According to Children's Hospital Boston, "There are no known factors or conditions that predispose an individual to the development of Diffuse Pontine Gliomas."
There are no known factors or conditions that predispose an individual to the development of diffuse pontine gliomas.
Diffuse pontine gliomas generally have a short duration (median 1 month) of symptoms prior to diagnosis, reflecting the rapid growth of these tumors. The following are the most common DIPG symptoms, however each child may experience symptoms differently. Common symptoms may include:
DIPG symptoms may resemble other conditions or medical problems. Always consult your child’s physician for a diagnosis.
In order to diagnose Diffuse Pontine Glioma, a physician will conduct a physical examination and administer the following tests:
Gliomas are heterogeneous tumors that are classified according to their most aggressive appearing elements. The World Health Organization classification scheme includes 4 grades of glioma. The pathological grade of diffuse pontine gliomas is not always established. Only 25-30 percent of these tumors are biopsied. Their clinical course is most consistent with their being the most aggressive form of astrocytic tumor or the grade IV glioblastoma multiforme. These tumors are characterized as being of astrocytic origin but having increased numbers of cells (hypercellularity), abnormal cells and nuclei (cytologic and nuclear atypia), increased proliferation of cells (mitoses), increased cell death (necrosis) and increased growth of blood vessels (vascular endothelial proliferation). These are aggressive tumors that infiltrate adjacent normal brain tissue and have a significant tendency to spread outside of the central nervous system.
A diagnosis of diffuse pontine glioma is most commonly made from characteristic radiologic studies. The location of these tumors and their tendency to diffusely infiltrate normal tissue makes biopsy a high-risk procedure. Biopsies have been performed when the symptoms and other tests do not seem typical for diffuse pontine glioma. Diagnostic procedures for diffuse pontine glioma may include:
computerized tomography scan (also called a CT or CAT scan) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. CT scans are more detailed than general x-rays.
A CT scan can assess the density of tumor tissue, compared to normal brain tissue, as well as establish its mass effect (the effect of an additional space occupying mass within the closed cavity of the skull on the normal brain). Diffuse pontine gliomas most often appear as round masses that expand the pons. When intravenous dyes are injected, these tumors avidly absorb dye and therefore are referred to as enhancing lesions
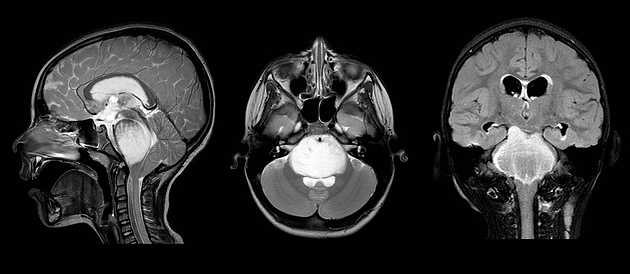
magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. MRI provides greater anatomical detail than CT scan and can better distinguish between tumor, tumor-related swelling and normal tissue. The typical MRI appearance of a diffuse pontine glioma is a round mass that expands the pons. When intravenous dye is administered, it displays a ring of enhancement. There can be growth up or down the brainstem, axial growth, or growth forward or backward out of the brainstem, exophytic growth.
magnetic resonance spectroscopy (MRS) - a test done along with MRI at specialized facilities that can detect the presence of particular organic compounds produced by the body's metabolism within sample tissue that can identify tissue as normal or tumor, and may be able to distinguish between glial tumors and tumors of neuronal origin.
Specific DIPG treatment will be determined by your child's physician based on:
DIPG Treatment may include:
Conventional limited field radiation produces responses in 75 percent of patients with diffuse pontine gliomas. These responses are short-lived however, with a median duration of less than 6 months. Several trials to increase the dose have been performed and none has improved survival.
There is no surgical option in the treatment of these tumors. Experimental chemotherapy delivered concurrent to radiation therapy is actively being investigated in the treatment of diffuse pontine gliomas. Several trials evaluating new agents such as thalidomide and temazolamide are either underway or recently completed. In addition, there are trials evaluating whether improved response to traditional chemotherapeutic agents may be obtained via novel delivery systems to more directly introduce the drugs into the brain. Data on the efficacy of these regimens should be available soon. To date, no chemotherapy regimen has been demonstrated to increase survival in diffuse pontine gliomas.
As with all pediatric cancers, care should be delivered at specialized centers where multidisciplinary teams can provide not only expert diagnostics and experienced medical, surgical and radiation oncologists, but also psychosocial support, neuro-psychological testing and specialized school plans, all delivered in a child- and family-sensitive and friendly environment.
Side effects of DIPG treatment may arise from radiation and chemotherapy. Radiation therapy often produces inflammation, which can temporarily exacerbate symptoms and dysfunction. To control this inflammation steroids are sometimes necessary.
Some of the chemotherapy agents are associated with fatigue, diarrhea, constipation and headache. These side effects can be effectively managed under most circumstances with standard medical approaches.
Many specialized brain tumor treatment centers have now added staff who are experts in complementary or alternative medicine. These treatments, including acupuncture/acupressure, therapeutic touch, massage, herbs and dietary recommendations, can also help to control pain and side effects of therapy.
The prognosis for diffuse pontine gliomas remains poor. Median survival is less than 1 year and the 2-year survival rate is less than 20 percent.
Clinical trials and experimental therapies are available for patients with relapsed high-grade gliomas at specialized centers. Current trials include novel medications as well as new methods for the delivery of more traditional agents.